About Low Grade Gliomas
The most common form of low-grade brain tumour is a group of tumours known as ‘Low-Grade Gliomas’ or ‘LGGs’. The brain contains about 40 billion nerve cells, known as neurons, which are held in place and supported by glial cells. Glioma is a general name for tumours that develop from these glial cells, the supportive tissue of the brain. Tumour types are named after the cells from which they arise.
Types of Tumour
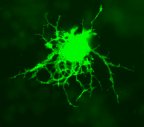
 Astrocytomas develop from astrocyte cells (see image, right). Astrocytes are three dimensional star-shaped cells which form a network around neurons, and are now thought to be involved in almost all aspects of brain function. They have a critical role in maintaining the right environment in your brain, so that the neurons can function properly. For example, astrocytes are thought to play an important role in keeping the synapses (small gaps across which chemical information is passed) between neurons functioning correctly. Astrocytes generate chemical signals sometimes called ‘gliotransmitters’, which can inhibit, stimulate, or fine-tune the messages passed between neurons. Each astrocyte may interact with several neurons and hundreds to thousands of synapses to integrate information effectively. In addition, the ‘feet’ of astroyctes connect to blood vessels in the brain, and by signalling blood vessels to expand or narrow, astrocytes also regulate local blood flow to provide oxygen and nutrients to neurons. There is growing evidence that astrocytes can even alter how a neuron is built, by directing where to make synapses or dendritic spines. They can also attract new cells to their territory (like immune cells and perhaps even adult neural stem cells) to repair any damage.
Astrocytomas develop from astrocyte cells (see image, right). Astrocytes are three dimensional star-shaped cells which form a network around neurons, and are now thought to be involved in almost all aspects of brain function. They have a critical role in maintaining the right environment in your brain, so that the neurons can function properly. For example, astrocytes are thought to play an important role in keeping the synapses (small gaps across which chemical information is passed) between neurons functioning correctly. Astrocytes generate chemical signals sometimes called ‘gliotransmitters’, which can inhibit, stimulate, or fine-tune the messages passed between neurons. Each astrocyte may interact with several neurons and hundreds to thousands of synapses to integrate information effectively. In addition, the ‘feet’ of astroyctes connect to blood vessels in the brain, and by signalling blood vessels to expand or narrow, astrocytes also regulate local blood flow to provide oxygen and nutrients to neurons. There is growing evidence that astrocytes can even alter how a neuron is built, by directing where to make synapses or dendritic spines. They can also attract new cells to their territory (like immune cells and perhaps even adult neural stem cells) to repair any damage.
Source of image: Wikimedia Commons
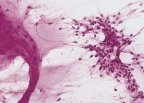
 Oligodendrogliomas develop from oligodendrocytes (see image, right). These are cells that wrap tightly around axons (the parts of neurons which look like ‘arms’) to form the myelin sheath. The myelin sheath speeds up the electrical communication signal that travels down an axon.
Oligodendrogliomas develop from oligodendrocytes (see image, right). These are cells that wrap tightly around axons (the parts of neurons which look like ‘arms’) to form the myelin sheath. The myelin sheath speeds up the electrical communication signal that travels down an axon.
Source of image: Wikimedia Commons
 Ependymoma cells line the ventricles of the brain (ventricles being the hollow spaces in your brain that contain cerebrospinal fluid), the central canal of the spinal cord, and the filum terminale (a thread-like structure within the lower end of the spinal cord).
Ependymoma cells line the ventricles of the brain (ventricles being the hollow spaces in your brain that contain cerebrospinal fluid), the central canal of the spinal cord, and the filum terminale (a thread-like structure within the lower end of the spinal cord).
For extensive information about Ependymomas, you may like to visit the website of the American based CERN Foundation (Collaborative Ependymoma Research Network).
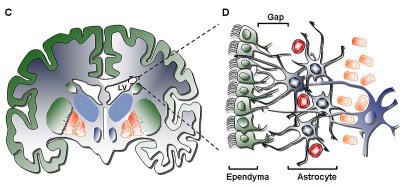
Source of Image: Wikimedia Commons
All low-grade gliomas are primary brain tumours, meaning that they begin within cells found only in the brain and can not spread to other parts of the body. They usually affect young people, the median age of symptom onset being 35 years, and the most common way to present is with an epileptic seizure.
The term ‘Low-Grade’ refers to the definition given by the WHO (World Health Organisation) grading system for brain tumours. WHO Grades I and II are both considered to be low-grade brain tumours, Grade I being found mainly in children and Grade II mainly in adults. Essentially, these two lower grades indicate that a tumour has cells that are dividing slowly, and therefore that the tumour as a whole is growing slowly.
Grade I tumours rarely progress to a higher grade, whether they are found in children or adults.
Grade II tumours can sometimes transform to a higher grade, but the reasons why this happens are not understood, and therefore it is not possible to predict a timescale, nor give an indication or risk, for individual patients. This uncertainty is one of the greatest challenges of living with a low-grade brain tumour.
WHO Grades III and IV indicate a high-grade Brain Tumour in which cells are dividing rapidly, and therefore a tumour that is growing more quickly.
Table 1. List of Low Grade Glioma (LGG) and High Grade Glioma (HGG) Classification
| Gliomas | WHO Grade | Grouping |
|---|---|---|
| Astrocytic tumours | ||
| Diffuse Astrocytoma | 2 | LGG |
| Anaplastic astrocytoma | 3 | HGG |
| Glioblastoma | 4 | HGG |
| Pilocytic astrocytoma | 1 | LGG |
| Pleomorphic xanthoastrocytoma | 2 | LGG |
| Subependymal giant cell astrocytoma | 1 | ‘LGG |
| Oligodendroglial tumours | ||
| Oligodendroglioma | 2 | LGG |
| Anaplastic oligodendroglioma | 3 | HGG |
| Mixed gliomas | ||
| Oligoastrocytoma | 2 | LGG |
| Anaplastic oligoastrocytoma | 3 | HGG |
| Ependymal tumours* | ||
| Ependymoma | 2 | LGG |
| Anaplastic ependymoma | 3 | HGG |
| Myxopapillary ependymoma | 1 | LGG |
| Subependymoma | 1 | LGG |
* Although classified as gliomas, ependymomas are uncommon idiosyncratic circumscribed tumours that are regarded clinically and therapeutically as distinct from gliomas of astrocytic or oligodendroglial lineage. There is also uncertainty about the clinicopathological value of distinguishing between classic (WHO grade 2) and anaplastic (WHO grade 3) ependymomas.
Source: NICE Guidelines – Improving Outcomes for People with Brain and Other CNS Tumours, June 2006. Table 1. Based on World Health Organization classification of tumours. Kleihues P, Cavenee WK (2000) Pathology and Genetics of Tumours of the Nervous System. Lyon: IARC Press.
Classifying your brain tumour
It is sometimes difficult to tell exactly what type of brain tumour you have simply by studying a brain scan, so a definite diagnosis is not considered possible until a tumour sample can be assessed by a pathologist. Therefore your Consultant may recommend that you undergo surgery to enable him or her to take a biopsy from your tumour (if it is in an accessible part of the brain) so that the type and grade of tumour can be confirmed by studying the cells under a microscope.
Having a biopsy will mean a hospital stay, as it is done under general anaesthetic. First, a CT or MRI brain scan is done to find the exact position of the tumour. During the operation a small hole, called a burr hole, is made in the skull. A fine needle is then passed down through the burr hole to remove tiny pieces of the tumour, which are then sent to the laboratory and examined by the pathologist under a microscope. Only once cells have been studied under a microscope can the tumour be accurately diagnosed. The grade and tumour type will then be used to decide which type of treatment is most suited to your particular situation; options usually include surgery, radiotherapy and/or chemotherapy.